HIPAA violations can lead to various consequences, like financial penalties. This article covers the top 12 HIPAA violation examples, from data breaches to overprivileged access. It will help you understand what needs to be avoided and stay HIPAA compliant.
Managing sensitive healthcare information is important, but you might face certain challenges as an IT manager. These challenges include a lack of compliance training for employees, outdated security controls, snooping on healthcare records, etc., which can lead to accidental or intentional violations.
The consequences of such violations can be severe, including hefty fines, loss of trust, reputational damage, and more. Addressing these issues often involves managing the fallout, identifying gaps, and implementing preventive measures—all of which can be time-consuming and costly for your team.
The first step in managing this is awareness. You can educate your employees on what not to do, reduce risks, and strengthen your organization’s security by going through several HIPAA violation examples. Let’s discuss the various examples of HIPAA violations in detail.
12 HIPAA Violation Examples With Real Cases
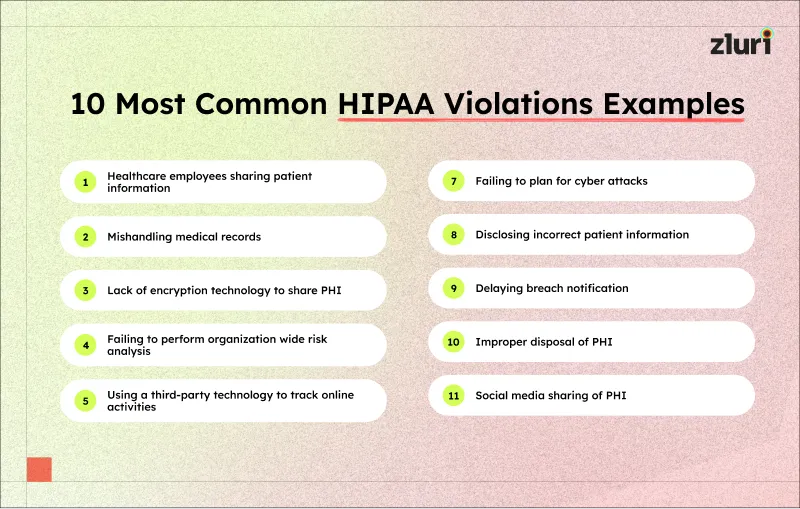
Here’s a list of various HIPAA violation examples.
1. Healthcare employees sharing patient information
One of the common HIPAA violation examples is when healthcare employees share patient information inappropriately. Under HIPAA’s Privacy Rule, all patient information must remain confidential. This rule restricts employees from discussing or sharing patient details without proper consent. However, lapses still happen.
These actions, even if accidental, violate HIPAA guidelines. Exposing patient information poses serious risks, such as patients losing trust in your organization, facing violation fines, and legal issues.
Case: According to a United States Attorney’s Office report, five former employees of Methodist Hospital and Roderick Harvey, a former employee of Memphis, were found guilty of unlawfully disclosing Methodist patients’ information.
From 2017 to 2020, Harvey paid the employees of Methodist Hospital to unlawfully provide patient names and phone numbers of those involved in car accidents, which he later sold to personal injury attorneys and chiropractors.
This breach portrays the serious legal consequences of mishandling sensitive health information, as HIPAA violations can result in imprisonment, hefty fines, and supervised release.
2. Mishandling medical record
When healthcare employees don’t secure patient data, they expose sensitive information to unnecessary risks. This, one of the prominent HIPAA violation examples, happens in many ways, such as storing data on unencrypted devices or sharing login credentials with unauthorized individuals. These actions can compromise your organization’s patient privacy and break HIPAA’s security rules.
In these, one of the common HIPAA violation examples, patients may lose trust, legal actions may follow, and your organization may face costly fines. However, this violation can be prevented by implementing strong access controls and data encryption.
Case: The U.S. Department of Health and Human Services’ Office resolved a HIPAA violation case at Yakima Valley Memorial Hospital in 2018. The hospital faced a HIPAA investigation after 23 security guards improperly accessed the medical records of 419 patients without a job-related reason.
This breach involved sensitive data like names, addresses, medical record numbers, and treatment notes, violating HIPAA’s Privacy and Security Rules. To resolve this, the hospital agreed to pay $240,000, updated its policies, trained its workforce, and strengthened safeguards against unauthorized access.
3. Lack of encryption technology to share PHI
Encryption technology will help you ensure that sensitive data stays secure, even if intercepted. Without it, one of the unintentional HIPAA violation examples, Protected Health Information (PHI) might be vulnerable to unauthorized access, theft, and misuse. This might risk your patient’s privacy and expose your organization to hefty violation penalties.
For example, imagine a healthcare provider emailing patient records to a third-party lab without encryption. If a hacker intercepts this email, they can easily read the PHI, including diagnoses, treatment details, and personal identifiers. Such an incident violates HIPAA’s Security Rule, which mandates appropriate measures to protect electronic PHI during transmission.
Thus, implementing encrypted email systems, secure file-sharing platforms, and training your employees to use them can prevent such violations. Taking these measures will ensure that the PHI remains secure and confidential.
Also Read: Examples of PHI
4. Failing to perform organization-wide risk analysis
Risk analysis is important in your organization to identify vulnerabilities in how the PHI is managed. Without this, being one of the common HIPAA violation examples, it will be difficult for healthcare entities to understand the threats to patient data. This lack of insight might increase the risk of breaches and non-compliance.
As per the standard, HIPAA's security rule requires covered entities to conduct regular risk assessments to address the concerns. Thus, conducting regular risk analysis helps you identify potential risks before they escalate, avoiding violations.
Case: In 2019, the U.S. Department of Health and Human Services Office announced that Medical Informatics Engineering, Inc. (MIE) has agreed to pay $100,000 and implement a corrective action plan. This settlement came after the company failed to perform a comprehensive risk analysis, potentially violating HIPAA Privacy and Security Rules.
5. Using a third-party technology to track data
One of the common HIPAA violation examples is that many large healthcare organizations use third-party tools to track data and other online activities without considering their security standards. This can lead to HIPAA violations, putting patient data at risk of identity theft, user harassment, data leaks, etc.
Case: According to a report by The Markup, a concerning practice among U.S. hospitals was revealed. Out of Newsweek's top 100 hospitals, 33 were found using a tracking tool called Meta Pixel. This tool sends data to Facebook whenever a user clicks to schedule a doctor's appointment.
Moreover, the information shared with Facebook included sensitive and identifiable health details. It captured data about medical conditions, prescriptions, and appointments, all linked to users' IP addresses. So, all the personal health information was shared with a third party without any security measures being taken.
6. Failing to plan for cyber attacks
Healthcare organizations generally handle a lot of sensitive patient data. Without proper planning, these data might be exposed to hackers. However, HIPAA’s Security Rule requires covered entities to assess risks and implement prevention measures. Avoiding this can lead to data and security breaches.
Imagine a healthcare organization that faced a ransomware attack. Without a plan, it would be challenging for your team to handle the cyber attack. In this case, hackers would access PHI, including patient names, medical histories, and social security numbers. This breach would violate the HIPAA rule and cause financial and reputational harm to the organization.
7. Disclosing incorrect patient information
Sharing incorrect patient information can lead to severe HIPAA violations. This, one of the common HIPAA violation examples, happens when healthcare organizations fail to verify the recipient or the details of the information being shared. Such errors can compromise patient privacy and lead to serious consequences.
For instance, consider a healthcare organization that accidentally sent the billing statements to the wrong address. These statements included patient names, account numbers, and treatment details. Now, this incident will breach the patient’s trust and result in regulatory scrutiny.
What should the organization do?
The organization needs to report the breach, notify affected individuals, and implement measures to prevent similar errors.
8. Delaying breach notification
As per the HIPAA Breach Notification Rule, you must cover the entities to notify impacted individuals, the Department of Health and Human Services (HHS), and, in some cases, notify the media within 60 days of discovering a breach. If the notification gets delayed in this process, then it violates the law and puts the patient's information at a higher risk of misuse, such as identity theft or fraud.
Case: According to The HIPAA Journal, Oklahoma State University—Center for Health Sciences (OSU-CHS) reported a data breach on January 5, 2018. This involved unauthorized access to a web server containing the electronic protected health information (ePHI) of 279,865 individuals.
The breach was initially believed to have occurred on November 7, 2017, but it was later revealed that it had started on March 9, 2016. The delay in notifying affected individuals and the Department of HHS was deemed a violation of HIPAA rules.
Therefore, as part of the resolution, OSU-CHS agreed to pay $875,000, implement a comprehensive corrective action plan, and undergo a two-year monitoring period.
9. Improper disposal of PHI
Both physical and digital records of PHI must be handled carefully to prevent unauthorized access. Otherwise, sensitive patient data can be exposed, leading to privacy breaches.
Thus, to prevent this, one of the uncommon HIPAA violation examples, you must ensure that all physical records are shredded or incinerated before disposal. Also, digital PHI must be securely erased using specialized tools to make it unrecoverable.
Case: In 2022, the OCR settled a case with New England Dermatology P.C. (NEDLC) over improper disposal of protected health information (PHI), resulting in a $300,640 fine and a corrective action plan.
In May 2021, NEDLC reported that specimen containers labeled with PHI, including patient names, birth dates, and sample details, were discarded in a parking lot garbage bin. OCR's investigation found violations of the HIPAA Privacy Rule, including unauthorized disclosure and inadequate safeguards for PHI protection.
10. Social media sharing of PHI
Multiple organizations use social media platforms for marketing or communication purposes. However, sharing patient data, even unintentionally, can lead to heavy penalties under HIPAA’s privacy rule. Moreover, PHI should never be shared on social media without proper authorization.
Case: In June 2021, former nurse Kelly Morris posted TikTok videos joking about mistreating patients, claiming they were harmless comedy skits. However, her employer, The Citadel at Winston-Salem, suspended her for unprofessional use of social media, stating her actions violated their core values.
While the videos did not reveal identifiable patient information, they displayed negligence and inappropriate behavior. As a result, Morris faced suspension and legal action, highlighting the risks of social media misuse in healthcare settings.
11. Stolen items like devices
One of the most prevalent HIPAA violation examples is the acquisition of mobile equipment with patients’ personal information. Due to the level of privacy intrusion, strong measures must be taken against people who steal PHI-containing devices such as laptops, smartphones, or USB drives.
For instance, a healthcare provider employee can log into a patient chart through a stolen laptop. If the device is not password-protected or encrypted, the person who finds the laptop can access sensitive information. Such behavior disregards privacy and breaches HIPAA security provisions.
In return, this organization may be subjected to severe sanctions in terms of fines. The organization will have to pay for losing patient confidence and a tarnished image. Thus, it is important to introduce encryption policies and efficient multi-factor authentication measures to prevent violations caused by thefts.
12. Discussing information over the phone
One of the unintentional HIPAA violation examples you may not think of is carelessly communicating over the phone. Even mentioning one piece of patient information without proper measures can easily lead to the unauthorized use of protected health information (PHI). This is a direct breach of HIPAA’s privacy regulation policies, as the patient information is supposed to be confidential.
Let’s say one of the employees needs to discuss a patient’s diagnosis and treatment plan over the phone and go to a public space, e.g., the lobby of a hospital/ cafeteria. Naturally, a lot of people hear this discussion, including the name of the patient, are included in such conversations. The fact that PHI is exposed is a serious violation of HIPAA.
These privacy impacts on patients and their information could lead to legal actions and financial penalties for the organization. In relation to such violations, fines are proportional to the degree of damages as well as to whether the organization exercised due diligence to prevent them.
How One Can Avoid HIPAA Violations?
In order to avoid HIPAA violations, follow the below mentioned ways:
- You can conduct self-audits that will help you quickly identify and remediate gaps.
- You need to document all your policies and procedures to support the investigators in meeting HIPAA compliance.
- Provide regular training on your policies and procedures, cybersecurity best practices, and more to make them aware of the violations and how to prevent them.
- Ensure all vendors handling the PHI sign Business Associate Agreements (BAAs) to confirm their compliance.
- Establish incident detection and response plans to minimize damages and recovery time from the incidents.
Ensure Compliance by Avoiding HIPAA Violations
Once you have understood the various HIPAA violation examples, the next step is to focus on preventing them and staying HIPAA compliant. However, achieving compliance will require more than just policies; it demands for proactive monitoring and timely action.
For instance, employees with unnecessary access to sensitive patient data can increase the risk of violations. You need a solution to review access regularly and act accordingly to manage this. However, to do so, you will need a platform like Zluri.
Zluri offers an access review platform that helps with reviewing users’ access and provides clear insights into who has access to your systems and data. With these insights, Zluri allows you to remediate overprivileged access, ensuring the right access to the right tool at the right time.
Also, Zluri provides access review reports that act as evidence that proper actions are taken to prevent HIPAA violations and stay compliant.
Let’s take JumpCloud as an example to see how you can automate the access review in Zluri.
Also Read: To stay compliant with HIPAA regulations, consider reading the HIPAA compliance checklist.
Frequently Asked Questions (FAQs)
1. What are HIPAA criminal penalties?
An individual who intentionally obtains or discloses identifiable health information in violation of the Privacy Rule may face a criminal penalty of up to $50,000 and up to one-year imprisonment.
2. What are the 4 levels of HIPAA financial penalties?
Here are the 4 levels:
- Tier 1: Lack of knowledge
- Tier 2: Reasonable cause and not willful neglect
- Tier 3: Willful neglect, corrected within 30 days
- Tier 4: Willful neglect, not corrected within 30 days
3. What are HIPAA's security policies?
The HIPAA Security Rule requires physicians to protect patients' electronically stored, protected health information ("ePHI") using appropriate administrative, physical, and technical safeguards. This will ensure the confidentiality, integrity, and security of this information.
4. What is a security risk in a healthcare facility?
Security risks involve theft of patient and employee data, extortion by encrypting data or disabling systems, hacktivists attacking a healthcare facility's reputation through online vandalism and by disclosing company records, and employee negligence, such as losing a laptop or forgetting to encrypt an email.





.svg)


























.webp)







.webp)
.webp)





.webp)